Going through rehab for substance abuse disorder doesn’t mean you’ll go through a lengthy process of staying sober without any medication. Most treatment programs involve a combination of behavioral and medicinal solutions to accommodate you in your recovery. However, there is an added danger of going back to old habits if you don’t commit to your treatment. For example, some medication meant for your withdrawal can also disrupt your sobriety by replacing it with a new addictive substance. This can cause you to undo your progress and prolong your recovery time. One drug that’s used for opioid recovery is Suboxone.
Reiterating Suboxone’s purpose
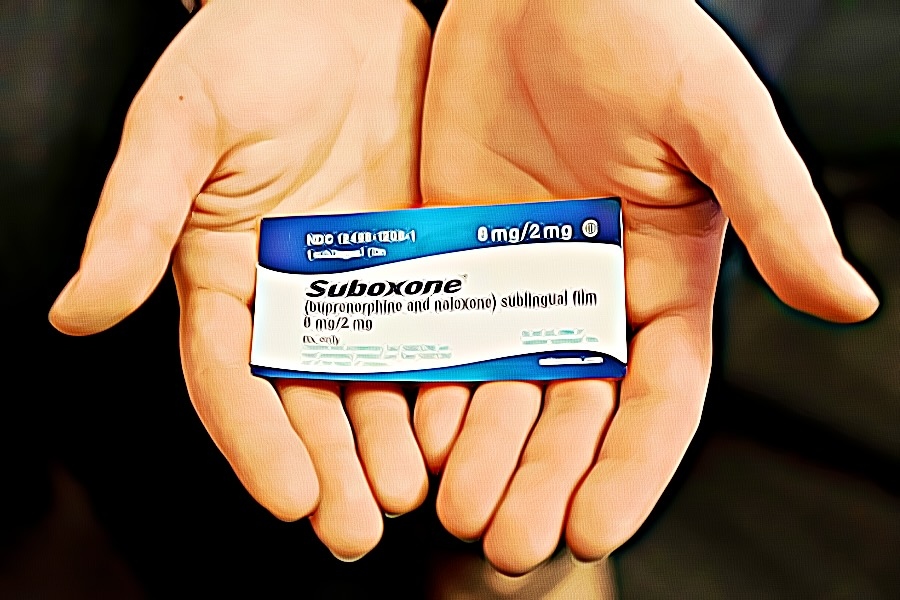
Suboxone is an infused combination of two drugs: buprenorphine and naloxone. It blocks the effects of opioid medication, allowing recovering patients to overcome their opiate addiction. Unfortunately, misuse of it can also lead to drug dependence. Because of this, you may need to request a different treatment plan for your suboxone addiction.
Since it’s a prescription medication, the primary way of abusing the drug is by procuring it from law addiction centers. These transactions can come illegally from patients who sell their medicine to others for cash. Studies note that Suboxone is sold primarily in the northeast region of the US. Although most people use it recreationally, some individuals purchase it illegally through a form of self-treatment. However, it’s important to note that treating yourself for opioid addiction without a physician’s diagnosis won’t be an effective solution.
Determining the right dosage for Suboxone
When you enter yourself into a rehab facility for opioid addiction recovery, your physician will consider three main factors for the suboxone dosage you’ll receive. First, they’ll check the severity of your opioid dependence based on the kinds of substances you’ve been using. Next, you’ll have an adjusted combination of Suboxone depending on your treatment stage. Finally, accounting for other medical conditions will finalize how much of the drug your body can handle.

Generally, your doctor will start you with a low dose and progressively adjust it over time while noting your improvement. Since Suboxone is made up of buprenorphine and naloxone, the dosage you’ll receive will be a ratio of both. Its potency will start with 2mg of buprenorphine with 0.5mg of naloxone. It can jump to 12 mg of buprenorphine and 3mg of naloxone.
Taking suboxone strips
Suboxone is only purchasable as an oral film that patients ingest sublingually through the cheek or through buccal means from the inside of your cheek. However, the two components of the drug, buprenorphine, and naloxone, come in different forms like tablets, skin patches, and even through a syringe.
Taking Suboxone pills
Similar to suboxone strips, suboxone pills are also taken in sublingually. When taking suboxone pills, it’s important to avoid swallowing, cutting, or chewing them. It’s best to let the medicine dissolve over time inside a patient’s mouth.
Understanding suboxone’s side effects
Using Suboxone as medication can cause anything from minor to serious side effects. Some typical side effects include general weakness, fatigue, sweating, and headaches. Besides these physical symptoms, Suboxone can also induce constipation, insomnia, anxiety, and depression. Since many patients take Suboxone to mitigate the side effects of other opioids, they tend to prefer these symptoms over the latter. Unfortunately, these side effects can reach extreme levels for people abusing their use of the drug.
Taking Suboxone with alcohol or benzodiazepines can cause an allergic reaction, leading to a swelling in the throat that causes difficulty breathing. Additionally, long-term abuse of the drug can cause liver damage or induce a fatal coma. This is why it’s important to be mindful of using Suboxone in the right doses.
People who misuse their suboxone medication can suffer a serious risk of opioid-based overdose. This manifests in symptoms such as anxiety, blurred vision, dizziness, fatigue, and even loss of consciousness. The danger of fainting while suffering from an overdose is the complication of respiratory depression, which can stop your breathing while you’re asleep, leading to brain damage, coma, or even death.
Experiencing suboxone withdrawal
When your body starts expelling Suboxone out of your system, you will experience several physical and psychological symptoms while under detox. Listed below are some physical signs you should expect when undergoing suboxone withdrawal:
- Feelings of intense heat or coldness throughout your body
- Skin abnormalities like prickling sensations or goosebumps spontaneously
- Muscle cramps leading to pain and discomfort
- Irregular sweating and night sweats due to Suboxone’s dehydrating properties
- Vomiting and diarrhea to expel Suboxone
- A general feeling of fatigue
Besides the physical symptoms above, your body can also respond to chemical imbalances through psychological responses. Listed below are several behavioral changes you should expect when undergoing suboxone withdrawal:
- Insomnia and other causes of irregular circadian rhythm
- Lack of appetite
- Increased drug cravings
Understanding the myths of Suboxone high
Although Suboxone provides a less impactful effect than other opiates, it can still significantly affect the user since it’s a partial agonist. As a Schedule III drug, the Drug Enforcement Administration (DEA) classifies it as a substance that inflicts low to moderate drug dependence potential. This makes it relatively easy for Suboxone users to be addicted to it.
Besides the dosage options above, people can also snort or inject Suboxone to experience a high. Although it’s an opioid, Suboxone cannot make its users high. However, its misuse with other narcotics is what makes it an addictive drug. People with substance abuse disorder use it as a temporary remedy to alleviate withdrawal symptoms from other opioids. With the minor drawback of experiencing mild side effects, they can maintain their dependence on other drugs.
Since Suboxone is a drug misused for improper self-treatment, it can cause dangerous combinations with other addictive substances. For example, using Suboxone with heroin will not deliver an increased high. However, mixing Suboxone with methadone and other similar compounds could make a deadly combination of symptoms. This increases the risk of using Suboxone considerably and can even lead to overdose death.
Analyzing how long Suboxone stays in your system
People who take Suboxone as a prescription medication need to understand how its half-life will affect the drug’s stay in your system. Its main ingredient of buprenorphine has a considerably longer elimination half-life than other opioids. It can remain detectable for 24 to 42 hours, depending on the dosage. Afterward, your body will take two full days before expelling around 50% of the buprenorphine contained in every dose of Suboxone.
For Suboxone to fully leave your body per dose, it takes up to nine days before it clears itself. However, your body must first break down buprenorphine by metabolizing it into a form called norbuprenorphine. This, in turn, has a half-life of over 150 hours, which means it’ll be detectable through your urine for over 14 days.
The other component of Suboxone, naloxone, has a much smaller half-life that lasts from 2 to 12 hours. It can also remain for up to 60 hours at most. Unlike buprenorphine, it’s not addictive, so doctors don’t have to test for people with naloxone exposure.
Conclusion
People should never feel ashamed about falling into the dangers of succumbing to another addiction. The process of recovery isn’t straightforward and universal for everyone. Facing hurdles are necessary if you want to achieve sobriety. Although the detox process and withdrawal experiences can seem challenging, you need to request immediate professional help. Otherwise, you risk experiencing more severe side effects and a prolonged suboxone withdrawal timeline.
Sources: